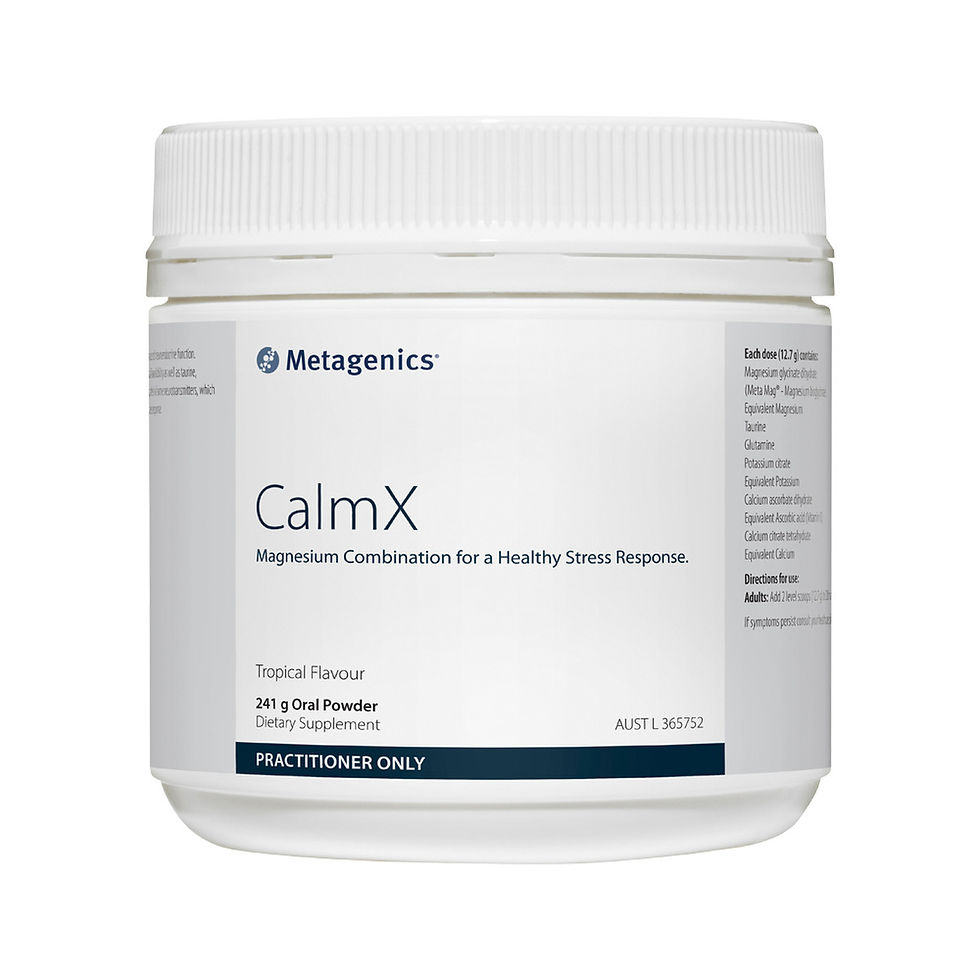
Metagenics
Calm X, Tropical
Nervous System Regulation
Provides 350mg of highly bioavailable Meta Mag® to relax the nervous system, and lower the stress response.
- Covalent bonding for superior absorption and fast clinical benefits
- Reduces Stress and Anxiety
- Indicated for Muscular tension and spasms
BECOME A MEMBER
SAVINGS $10.04 (inc. GST)
LOGIN
SIGN UP
QTY
BENEFITS
CLINICALLY PROVEN;
Nervous System Relaxant
Alleviates Stress and Anxiety
Reduces Muscle Aches, Pains, Cramps and Spasms
Modulates inflammatory responses
Migraine Prevention
Metabolic support
Lowers blood sugar
Reduces PMS symptoms
Reduces congentital abnormalitites in pregnancy
ANTISPASMODIC
Deficiency of magnesium is associated with muscular cramps, and magnesium has long been recognised for its important therapeutic applications in enhancing muscle relaxation and relieving spasm.[45]
Magnesium exerts its muscle-relaxing actions by competing with calcium for binding sites on troponin C, allowing the sarcoplasmic reticulum to actively transport calcium out of the sarcomere, thus inhibiting contraction and allowing relaxation.[46] Additionally, magnesium causes muscle relaxation by decreasing the amount of acetylcholine liberated at motor nerve terminals, reducing depolarisation and depressing the excitability of the muscle fibre membrane.[47]
Furthermore, magnesium is involved in the regulation of a wide variety of enzymatic reactions and phosphorylation-dependent processes essential for neuronal excitability. Therefore, magnesium is required for the correct muscle contractile signalling via motor neurons.
NEUROMUSCULAR SUPPORT
Amongst magnesium’s many vital roles is its importance in neuromuscular transmission. Magnesium prevents or controls convulsions by blocking neuromuscular transmission and decreasing the release of acetylcholine at the motor nerve terminals.[48] Magnesium deficiency should always be included in the differential diagnosis for a patient who presents with persistent or severe muscle pain.[49]
Both stress and hypomagnesemia potentiate each other’s negative effects.
Fibromyalgia (FM) is a particularly painful neuromuscular condition, which is most common among women aged 30 to 50.[50] This is a common syndrome characterised by long-term, body-wide pain and tenderness in the joints, muscles, tendons, and other soft tissues. The cause is unknown, but FM has also been linked to fatigue, sleep problems, headaches, and anxiety.[51] These same symptoms are also found in patients with low magnesium levels,[52] with red blood cell magnesium levels being found to be low in fibromyalgic patients.[53] People suffering from this condition tend to wake up with body aches and stiffness; with magnesium found to be effective in the reduction of these symptoms. The proposed mechanism of action is via mitochondrial support, as there is evidence of muscle hypoxia and deficient ATP production in FM.
Magnesium can also provide analgesic effects, due to its N-methyl-D-aspartate (NMDA) receptor blocking action.[54] Magnesium deficiency is particularly associated with increased susceptibility to painful migraines due to effects on neuroinflammation, NMDA receptor binding, glutamate and nitric oxide activity as well as serotonin receptor affinity.[55] Migraines have been linked to brain excitability, with magnesium able to block the excitatory NMDA glutamate receptors, thereby inactivating them.[56] Additionally, muscle cramps, muscle strains (and damage) and muscle tension are all associated with magnesium deficiency. Interestingly, approximately 70% of patients who have tension headaches also exhibit muscular tightness and tenderness. It is therefore no surprise that magnesium supplementation is of great benefit for patients presenting with tension-type headaches[57] and migraines.[58]
MODULATES INFLAMMATORY RESPONSES
Interestingly, it has been shown that after a few days of experimental magnesium deficiency in an animal model that clinical inflammatory syndrome is induced, characterised by leukocyte and macrophage activation, release of inflammatory cytokines and acute phase proteins, and excessive production of free radicals.[59]Research has led to the conclusion that increasing the extracellular magnesium concentration decreases the inflammatory response, while reduction of extracellular magnesium results in cell activation.[60]
Importantly, magnesium acts as a natural calcium antagonist, and the molecular basis for the inflammatory response is essentially the result of modulation of intracellular calcium concentration. The priming of phagocytic cells, the opening of calcium channels and activation of NMDA receptors, and the activation of nuclear factor kappa B (NFkB) have all been considered as potential mechanisms. Moreover, magnesium deficiency induces a systemic stress response by activation of neuro-endocrinological pathways. As nervous and immune systems interact bi-directionally, the role of neurological mediators, such as magnesium, have to be considered.[61]
Additionally, magnesium deficiency contributes to an exaggerated inflammatory response to immune stress, and oxidative stress is the consequence. Inflammation contributes to the pro-atherogenic changes in lipoprotein metabolism, endothelial dysfunction, thrombosis, and hypertension, and explains the aggravating effect of magnesium deficiency on the development of metabolic syndrome. Further studies are still needed to assess more accurately the role of magnesium in immune response in humans, but these experimental findings in animal models suggest that inflammation may be the missing link to explain the role of magnesium in many pathological conditions.[62]
METABOLIC SUPPORT
Hypomagnesaemia has been strongly related to type 2 diabetes mellitus (T2DM) due to magnesium’s many roles in insulin and glucose metabolism (Figure 5).[63] Intracellular magnesium regulates glucokinase (an enzyme which plays an important role in the regulation of carbohydrate metabolism),
In addition, chromium plays a significant role in glucose metabolism by potentiating the action of insulin.[64] For example, it facilitates insulin signalling by augmenting insulin binding through increasing the number of insulin receptors on cells.
Chromium also improves insulin sensitivity by increasing insulin receptor phosphorylation through modulation of kinase activity.[65] As such, it has important roles not only in glucose but also lipid metabolism. Signs of chromium deficiency in humans consuming standard diets include elevated serum glucose, insulin, cholesterol and triglycerides, and decreased high density lipoprotein (HDL) cholesterol.[66] Supplementation with chromium has demonstrated beneficial effects on people with conditions ranging from mild glucose intolerance to overt T2DM, without side effects.[67]
Hypomagnesaemia has been strongly related to type 2 diabetes mellitus due to magnesium’s many roles in insulin and glucose metabolism.
NERVOUS SYSTEM RELAXANT
Magnesium supplementation has been shown to affect all elements of the body’s reactions to stress, exerting a neuroprotective effect. For example, in the event of deficiency, magnesium repletion reverses the increased stress sensitivity, with pharmacological loading of magnesium inducing resistance to neuropsychological stressors such as glutamate[*] excitotoxicity.[68]
With the ability to inhibit the release of excitatory neurotransmitters, magnesium acts as a voltage-gated antagonist at the glutamate, NMDA receptor.[69] When the NMDA receptor is over-activated, it can result in increased cell death and increased excitotoxicity which ultimately results in neurological changes. For example, low levels of magnesium has been associated with hippocampal atrophy, with supplementation demonstrating the ability to boost brain derived neurotrophic factor (BDNF) and promote hippocampal neurogenesis.[70]Psychological stress is one of the states that can result in the release of glutamate (which exerts excitatory effects), and appears to be mediated, at least in part, via glucocorticoids, which can both increase glutamate levels and contribute to the neuronal damage.[71]
In a state of deficiency, the neuronal requirements for magnesium may not be met, causing the neuronal damage which can result in low mood.[72] Acute stress has been associated with increased plasma magnesium levels due to the release of stress hormones (catecholamines and corticosteroids), and increased urinary excretion.[73]This is due to the body shifting magnesium from the intracellular to extracellular space as a protective mechanism to reduce the effects of stress.[74] For example, by limiting the rate of inflammation and oxidation experienced at times of stress, as well as supporting extra neurotransmitter requirements.
With extended periods of stress resulting in progressively deficient magnesium levels, a vicious cycle can develop where stress increases cellular magnesium losses, thus resulting in an exaggerated stress response.[75] Moreover, magnesium deficiency is itself a stress to the body, as it has been linked to promoting catecholamine release, promoting proinflammatory factors, and disrupting sleep patterns.[76] Therefore, it is suitable to say that magnesium deficiency is both a cause and a consequence of stress.
The anxiolytic effects of magnesium are similarly attributed to the reduction of glutamate activity, and the increased actions of the gamma aminobutyric acid (GABA)-ergic systems[77] (Figure 6). This results in a soothing effect on the entire stress response system,[78] as GABA acts as the body’s primary calming influence, working to control and balance the effects of glutamate.
Magnesium ions regulate calcium ions as part of nerve cell conduction activity,[79] (Figure 7) with magnesium deficiency causing NMDA-coupled calcium channels to be biased towards opening, leading to further neuronal injury and neurological dysfunction.[80] This results in glutamate-induced neuro-excitotoxicity, which may manifest as anxiety and other mood and behavioural disorders.[81]
Magnesium is recommended as a migraine prophylactic for those suffering frequent migraines.
In addition, zinc is required throughout the human body for a myriad of chemical reactions necessary for normal body functioning.[83] For example, it is well-established that zinc supplementation provides antidepressant-like effects, with zinc deficient diets associated with low moods.[84] Zinc has been shown to increase BDNF, which is recognised as a target implicated in the aetiology of depression.[85] It has been demonstrated that BDNF plays a significant role in supporting patients with low mood, with a meta-analysis showing depressive patients have decreased serum and plasma BDNF levels.[86]
Zinc is highly concentrated in the synaptic vesicles of specific neurons, and regulates the release of neurotransmitters. The neurons that contain zinc are known as zinc-enriched neurons (ZEN), with cerebellar ZEN primarily associated with GABA neurotransmission, which produces a calming effect by balancing over-excitability. In other regions, ZEN are found in glutamate-producing neurons.[88] Furthermore, zinc has been shown to increase synaptic dopamine levels, thereby allowing dopamine to stay and engage with receptors longer within the synapse, and is considered an important regulator of dopamine transporter function.[89]
Zinc also acts as an inhibitory neuromodulator of glutamate release, regulating NMDA receptors.[90] The areas of the brain in which functional and structural changes occur in the course of low mood are areas of particularly high concentration of glutamatergic neurons sequestering zinc, and the subsequent NMDA receptors are characterised by a high degree of susceptibility to the inhibitory effects of zinc.[91] This reflects a further need for sufficient zinc to reduce the excitotoxicity associated with the pathophysiology of mood disorders.
Pyridoxine (vitamin B6) has many important roles; in its coenzyme form, pyridoxal phosphate (PLP), it is associated with over 100 enzymes, the majority of which are involved in amino acid metabolism.[92] Vitamin B6 is fundamental to the production of many neurotransmitters[93] and is specifically involved in the creation of histidine to histamine, tryptophan to serotonin, glutamate to GABA, and dihydroxyphenylalanine to dopamine,[94] as well as the synthesis of adrenaline and noradrenaline.[95] Therefore, deficiency in this nutrient is often associated with psychological disturbances such as mood alterations,[96] with signs of deficiency including confusion, lethargy and depression. Up to 40% of food-derived vitamin B6 can be lost with cooking.[97] P-5-P is the main circulating form exported from the liver and may be more beneficial with patients where conversion is compromised (e.g. liver disease or zinc or magnesium deficiency).[98],[99]
MUSCLE ACHES, PAINS, CRAMPS AND SPASMS
Magnesium is well known as an effective agent to reduce muscle cramps and spasms. In a double-blind randomised placebo-controlled trial on 73 women, it was found that otherwise healthy pregnant patients suffering with leg cramping had a negative magnesium balance.[100] Oral supplementation with three doses of 122 mg magnesium daily (one in the morning, two at night) for three weeks effectively reduced cramping in comparison to controls.[101]
Furthermore, non-pregnant volunteers suffering regular leg cramps were recruited into a randomised, double-blind, cross-over placebo-controlled trial.[102] They were given a supplement equivalent to 300 mg elemental magnesium and matching placebo for six weeks each. The number of cramps was recorded in cramp diaries, with the results showing fewer leg cramps were experienced when the patients received the active treatment of magnesium compared to placebo (Figure 8).[103]
MIGRAINE PREVENTION
Deficiency in magnesium is associated with neuronal dysfunction, such as found in those who suffer migraines.[105] Magnesium is recommended as a migraine prophylactic for those suffering frequent migraines,[106],[107] with the more bioavailable magnesium forms demonstrating increased efficacy compared to other low-absorbable forms.[108]
Several studies have demonstrated significant benefits in patients with the use of magnesium to prevent headaches and migraines. For example, in a double-blind, placebo-controlled trial in women experiencing menstrual migraine, the use of magnesium pyrrolidone carboxylic acid (360 mg/day) starting on the 15th day of their cycle until the next menses, resulted in a significantly reduced pain score, and a reduction in the number of days with headache.[109]
Further, in another double-blind randomised study, adults suffering migraines aged 18 to 65 years were given oral magnesium at a dose of 600 mg daily (as trimagnesium dicitrate) over 12 weeks.[110] The results demonstrated a substantial 41.6% decrease in migraine attack frequency, compared to only 15.8% in placebo group. Additionally, after three months of oral magnesium citrate (600 mg/day), patients experiencing migraines without aura showed notable reductions in migraine frequency (p=0.005) and severity (p<0.001),[111] further displaying the preventative effect of daily magnesium on the recurrence of debilitating migraines.
LOWERS BLOOD SUGAR
Hypomagnesaemia is a prominent feature of T2DM, with many studies having been performed to show the effects of magnesium supplementation on patients with prediabetes and diabetes. For example, a recent systematic review and meta-analysis of 18 randomised controlled trials concluded that magnesium supplementation can improve glucose parameters in people with diabetes, and also improves insulin-sensitivity parameters in those at high risk of T2DM.[112] Compared with placebo, magnesium treatment was shown to reduce fasting plasma glucose in those with diabetes, and improve plasma glucose levels after a glucose tolerance test in those at high risk of diabetes.
Additionally, a meta-analysis of 13 cohort studies with over 500,000 participants found a significant decrease in the incidence of diabetes with higher magnesium intake.[113] Moreover, a 2017 cohort study of 395 patients with T2DM showed 30.6% of patients suffered from hypomagnesaemia, with both plasma triglyceride (p<0.001) and actual glucose levels (p<0.001) negatively correlated with plasma magnesium concentration.[114] The patients in this study who were using metformin, proton pump inhibitors or β-adrenergic receptor agonists displayed even further reduced plasma magnesium levels.
Furthermore, the combination of magnesium with chromium has been shown to decrease IR more effectively than either alone.[115] One hundred and twenty subjects with IR were randomly divided to receive either placebo, chromium (160 µg/day), magnesium (200 mg/day) or chromium plus magnesium for three months. The results indicated the combination of chromium with magnesium improved the IR more effectively than either alone, with significant decreases in fasting serum glucose (0.37 mmol/L; p<0.01), fasting insulin (2.91 µIU/mL; p<0.01) and IR index (0.60; p<0.01) displayed in the combination group only. Additionally, significant changes in glucose-transporter-4 (2.9-fold increase; p<0.05) and glycogen-synthase-kinase-3β (2.2-fold decrease; p<0.05) mRNA levels in activated T-lymphocytes were observed with the combination of the two minerals, but not in the other groups.
A meta-analysis of 13 cohort studies with over 500,000 participants found a significant decrease in the incidence of diabetes with higher magnesium intake.
ALLEVIATES STRESS AND ANXIETY
Magnesium is highly associated with stress levels, and both stress and hypomagnesemia potentiate each other’s negative effects.[116] With extensive reviews performed on magnesium’s association alongside increased stress, Cuciureanu and Vink[117] suggest that magnesium should be evaluated in patients presenting with a variety of mental/emotional symptoms, including hyper-emotionality, generalised anxiety, panic attack disorders, insomnia, fatigue and asthenia. They further suggest that alleviation of clinical manifestations with oral supplementation of 5 mg/kg/day can confirm the diagnosis of suspected hypomagnesemia.
In humans, chronic sleep deprivation is associated with progressively decreasing levels of magnesium, with low magnesium being associated with decreased melatonin.[118] Additionally, experimental data indicates magnesium deficiency can lead to slightly increased plasma corticosterone levels, increased irritability, aggressive behaviour, disrupted sleep patterns and higher mortality rates in animal studies compared to controls.[119]
Chronic sleep deprivation is associated with progressively decreasing levels of magnesium, with low magnesium being associated with decreased melatonin.
Interestingly, magnesium and oxidative status were investigated in young military volunteers exposed to chronic stress (>10 years) or subchronic stress (>3 months).[120] Both of the stress situations caused a significant decrease (p<0.05) in total plasma magnesium, with chronic and subchronic stress causing significant decreases in ionised magnesium compared to the level of ionised magnesium in the control group. The findings of this study supports the need for magnesium supplementation in people living in conditions of stress. Additionally, this study shows that chronic stress of long duration but moderate intensity, as well as subchronic exposure to intense stress, can significantly alter magnesium homeostasis and initiate increased oxidative stress.
Additionally, zinc has been associated with numerous behavioural alterations in both humans and animals (Figure 5).[121] Notably, serum zinc levels have been correlated with severity of depression, with zinc supplementation used in the augmentation therapies as a treatment for depression.[122] It has been confirmed in multiple studies that the more severe the depressive symptoms in patients, the lower the serum zinc, compared to non-depressed controls.[123]
Animal studies of zinc deficiency show increased states of aggression and anxiety, with anxiety-like behaviours shown to develop within just two weeks of being fed a zinc-deficient diet.[124] The animal models of zinc deficiency have also demonstrated a lowered stress response, with lower zinc levels correlating to higher corticosterone levels following stress in comparison to controls, suggesting zinc to be an important factor in the modulation of anxiety and stress responses.
REPRODUCTIVE HEALTH
Another aspect of magnesium’s many roles is its impact on female health. Through its effects on energy production, neuromuscular function and inflammation, magnesium deficiency can be seen to contribute to premenstrual syndrome (PMS), infertility, and problems associated with pregnancy. Deficiencies of magnesium have been implicated in various reproductive events such as congenital anomalies, pregnancy-induced hypertension, placental abruption, premature rupture of membranes, still births and low birth weight.[125]
Pregnant women with hypomagnesaemia have been found to be 47 times more likely to experience pre-eclampsia than predicted by their BMI.
Pregnancy has been shown to induce a significant (15%) decrease in serum magnesium levels, due primarily to increased renal excretion. Pregnant women with hypomagnesaemia have been found to be 47 times more likely to experience pre-eclampsia than predicted by their body mass index (BMI).[126] In addition, vaginal (but not caesarean) delivery results in significant decreases in magnesium; most probably due to the participation of skeletal and uterine muscles during labour.[127]
Magnesium supplementation during pregnancy has been shown to improve maternal health and foetal outcome, and intravenous magnesium sulphate has been used as a tocolytic agent, to reduce uterine contractility in preterm labour.[128]
Additionally, magnesium and vitamin B6 have both been demonstrated to be beneficial for improving premenstrual mood of women, in isolation[129],[130] or combination.[131]Forty-four women (average age 32) were randomly assigned to take consecutively: 200 mg magnesium (as oxide), 50 mg vitamin B6, a combination of the magnesium and B6, or placebo for one menstrual cycle. The results showed a significant effect of the combination of 200 mg/day magnesium with 50 mg/day vitamin B6 on reducing anxiety-related premenstrual symptoms (nervous tension, mood swings, irritability, or anxiety) demonstrating that the synergistic effects of the nutrients were greater than the effect of the magnesium or B6 in isolation.[132]
INGREDIENTS
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
Item
Description
DIRECTIONS
Adults:
Add 2 level scoops (12.7 g) to 600 mL of water and drink progressively
EVIDENCE
References
[1] Australian Bureau of Statistics (ABS) [Internet]. Canberra (ACT): ABS; 2015. Australian Health Survey: Usual Nutrient Intakes 2011-12; 2015 Mar 6 [2017 Jan 13]. Available from: www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.008~2011-12~Main%20Features~Magnesium~406.
[2] Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
[3] Abumaria N, Yin B, Zhang L, Li X-Y, Chen T, Descalzi G, et al. Effects of elevation of brain magnesium on fear conditioning, fear extinction, and synaptic plasticity in the infralimbic prefrontal cortex and lateral amygdala. J Neurosci. 2011 Oct;31(42):14871-14881.
[4] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[5] Gommers LMM, Goenderop JGJ, Bindels RJM, de Baaij JHF. Hypomagnesemia in type 2 diabetes: a vicious circle? Diabetes. 2016 Jan;65:3-13.
[6] Gropper SS, Smith JL. Advanced nutrition and human metabolism. 6th ed. Belmont (CA): Wadsworth, Cengage Learning; 2013. p. 527-530.
[7] Facchinetti F, Borella P, Sances G, Fioroni L, Nappi RE, Genazzani AR. Oral magnesium successfully relieves premenstrual mood changes. Obstet Gynecol. 1991 Aug;78(2):177-181.
[8] Pathak P, Kapil U. Role of trace elements zinc, copper and magnesium during pregnancy and its outcome. Indian J Pediatr. 2004 Nov;71(11):1003-1005.
[9] Long S, Romani AMP. Role of cellular magnesium in human disease. Austin J Nutr Food Sci. 2015 Mar;2(10).
[10] Nechifor M. Magnesium in psychoses (schizophrenia and bipolar disorder). In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[11] Bohl CH, Volpe SL. Magnesium and exercise. Critical Reviews in Food Science and Nutrition. 2002;42(6):533-563.
[12] Australian Bureau of Statistics (ABS) [Internet]. Canberra (ACT): ABS; 2015. Australian Health Survey: Usual Nutrient Intakes 2011-12; 2015 Mar 6 [2017 Jan 13]. Available from: www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.008~2011-12~Main%20Features~Magnesium~406.
[13] Serefko A, Szopa A, Poleszak E. Magnesium and depression. Magnes Res. 2016;29(3):112-119.
[14] National Institutes of Health Office of Dietary Supplements [Internet]. ODS; 2016. Magnesium; 2018 Mar 2 [2018 Mar 5]. Available from: http://ods.od.nih.gov/factsheets/magnesium.asp.
[15] National Institutes of Health Office of Dietary Supplements [Internet]. ODS; 2016. Magnesium; 2018 Mar 2 [2018 Mar 5]. Available from: http://ods.od.nih.gov/factsheets/magnesium.asp.
[16] National Institutes of Health Office of Dietary Supplements [Internet]. ODS; 2016. Magnesium; 2018 Mar 2 [2018 Mar 5]. Available from: http://ods.od.nih.gov/factsheets/magnesium.asp.
[17] Graff D. Bioavailability of magnesium chelazome®Albion® Research Notes. 2000 Mar;9(1):2-3.
[18] Hartle JW, Morgan S, Poulsen T. Development of a model for in-vitro comparative absorption of magnesium from five magnesium sources commonly used as dietary supplements. FASEB Journal. 2016 Apr;128(6).
[19] Schuette SA, Lashner BA, Janghorbani M. Bioavailability of magnesium diglycinate vs magnesium oxide in patients with ileal resection. JPEN J Parenter Enteral Nutr. 1994 Sep-Oct;18(5):430-5. doi: 10.1177/0148607194018005430.
[20] Siebrecht S. Magnesium Bisglycinate as safe form for mineral supplementation in human nutrition. OM & Ernährung. 2013;144:2-16.
[21] Workinger JL, Doyle RP, Bortz J. Challenges in the diagnosis of magnesium status. Nutrients. 2018 Sep 1;10(9). pii: E1202. doi: 10.3390/nu10091202.
[22] Bortz J. Challenges with magnesium bioavailability studies, magnesium salts, chelates and caco2 cell uptake studies. Albion Laboratories. 2017 Feb.
[23] Siebrecht S. Magnesium Bisglycinate as safe form for mineral supplementation in human nutrition. OM & Ernährung. 2013;144:2-16.
[24] Hartle JW, Morgan S, Poulsen T. Development of a model for in-vitro comparative absorption of magnesium from five magnesium sources commonly used as dietary supplements. FASEB Journal. 2016 Apr;128(6).
[25] Workinger JL, Doyle RP, Bortz J. Challenges in the diagnosis of magnesium status. Nutrients. 2018 Sep 1;10(9). pii: E1202. doi: 10.3390/nu10091202.
[26] Thongon N, Krishnamra N. Apical acidity decreases inhibitory effect of omeprazole on Mg(2+) absorption and claudin-7 and -12 expression in Caco-2 monolayers. Exp Mol Med. 2012 Nov 30;44(11):684-93. doi: 10.3858/emm.2012.44.11.077.
[27] Thongon N, Krishnamra N. Omeprazole decreases magnesium transport across Caco-2 monolayers. World J Gastroenterol. 2011 Mar 28;17(12):1574-83. doi: 10.3748/wjg.v17.i12. 1574.
[28] Thongon N, Krishnamra N. Apical acidity decreases inhibitory effect of omeprazole on Mg(2+) absorption and claudin-7 and -12 expression in Caco-2 monolayers. Exp Mol Med. 2012 Nov 30;44(11):684-93. doi: 10.3858/emm.2012.44.11.077.
[29] Thongon N, Krishnamra N. Omeprazole decreases magnesium transport across Caco-2 monolayers. World J Gastroenterol. 2011 Mar 28;17(12):1574-83. doi: 10.3748/wjg.v17.i12. 1574.
[30] Bortz J. Challenges with magnesium bioavailability studies, magnesium salts, chelates and caco2 cell uptake studies. Albion Laboratories. 2017 Feb.
[31] Workinger JL, Doyle RP, Bortz J. Challenges in the diagnosis of magnesium status. Nutrients. 2018 Sep 1;10(9). pii: E1202. doi: 10.3390/nu10091202.
[32] Siebrecht S. Magnesium Bisglycinate as safe form for mineral supplementation in human nutrition. OM & Ernährung. 2013;144:2-16.
[33] Bortz J. Challenges with magnesium bioavailability studies, magnesium salts, chelates and caco2 cell uptake studies. Albion Laboratories. 2017 Feb.
[34] Workinger JL, Doyle RP, Bortz J. Challenges in the diagnosis of magnesium status. Nutrients. 2018 Sep 1;10(9). pii: E1202. doi: 10.3390/nu10091202.
[35] Siebrecht S. Magnesium Bisglycinate as safe form for mineral supplementation in human nutrition. OM & Ernährung. 2013;144:2-16.
[36] Schuette SA, Lashner BA, Janghorbani M. Bioavailability of magnesium diglycinate vs magnesium oxide in patients with ileal resection. JPEN J Parenter Enteral Nutr. 1994 Sep-Oct;18(5):430-5. doi: 10.1177/0148607194018005430.
[37] Supakatisant C, Phupong V. Oral magnesium for relief in pregnancy-induced leg cramps: a randomised controlled trial. Matern Child Nutr. 2015 Apr;11(2):139-45. doi: 10.1111/j.1740-8709.2012.00440.x.
[38] Workinger JL, Doyle RP, Bortz J. Challenges in the diagnosis of magnesium status. Nutrients. 2018 Sep 1;10(9). pii: E1202. doi: 10.3390/nu10091202.
[39] Schuette SA, Lashner BA, Janghorbani M. Bioavailability of magnesium diglycinate vs magnesium oxide in patients with ileal resection. JPEN J Parenter Enteral Nutr. 1994 Sep-Oct;18(5):430-5. doi: 10.1177/0148607194018005430.
[40] Bortz J. Physiology of magnesium absorption and challenges with analytic methods. Albion Laboratories. 2017 Feb.
[41] Bortz J. Challenges with magnesium bioavailability studies, magnesium salts, chelates and caco2 cell uptake studies. Albion Laboratories. 2017 Feb.
[42] Siebrecht S. Magnesium Bisglycinate as safe form for mineral supplementation in human nutrition. OM & Ernährung. 2013;144:2-16.
[43] Bortz J. Challenges with magnesium bioavailability studies, magnesium salts, chelates and caco2 cell uptake studies. Albion Laboratories. 2017 Feb.
[44] Hartle JW, Morgan S, Poulsen T. Development of a model for in-vitro comparative absorption of magnesium from five magnesium sources commonly used as dietary supplements. FASEB Journal. 2016 Apr;128(6).
[45] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 677-692.
[46] Rossier P, van Erven S, Wade DT. The effect of magnesium oral therapy on spasticity in a patient with multiple sclerosis. Eur J Neurol. 2000;7(6):741-744.
[47] Rossier P, van Erven S, Wade DT. The effect of magnesium oral therapy on spasticity in a patient with multiple sclerosis. Eur J Neurol. 2000;7(6):741-744.
[48] Akhtar MI, Ullah H, Hamid M. Magnesium, a drug of diverse use. J Pak Med Assoc. 2011 Dec;61(12)1220-1225.
[49] Bilbey DL, Prabhakaran VM. Muscle cramps and magnesium deficiency: case reports. Can Fam Physician. 1996 Jul;42:1348-1351.
[50] Abraham GE, Flechas JD. Management of fibromyalgia: Rationale for the use of magnesium and malic acid. J Nutr Med. 1992;3:49-59.
[51] Yunus MB, Masdi AT, Calabro JJ, Miller KA, Feigenbaum SL. Primary fibromyalgia (fibromyositis): clinical study of 50 patients with matched normal controls. Sem Arthritis Rheum. 1981;11:151-171.
[52] Romano TJ, Stiller JW. Magnesium deficiency in fibromyalgia syndrome. J Nutr Env Med. 1994;4(2):165-167.
[53] Abraham GE, Flechas JD. Management of fibromyalgia: Rationale for the use of magnesium and malic acid. J Nutr Med. 1992;3:49-59.
[54] Akhtar MI, Ullah H, Hamid M. Magnesium, a drug of diverse use. J Pak Med Assoc. 2011 Dec;61(12)1220-1225.
[55] Teigen L, Boes CJ. An evidence-based review of oral magnesium supplementation in the preventive treatment of migraine. Cephalalgia. 2015 Sep;35(10):912-22
[56] Teigen L, Boes CJ. An evidence-based review of oral magnesium supplementation in the preventive treatment of migraine. Cephalalgia. 2015 Sep;35(10):912-
[57] Altura BM, Altura BT. Tension headaches and muscle tension: is there a role for magnesium? Med Hypotheses. 2001;57(6):705-713.
[58] Sun-Edelstein C, Mauskop A. Role of magnesium in the pathogenesis and treatment of migraine. Expert Rev. Neurother. 2009;9(3):369-379.
[59] Mazur A, Maier JA, Rock E, Gueux E, Nowacki W, Rayssiguier Y. Magnesium and the inflammatory response: potential physiopathological implications. Arch Biochem Biophys. 2007 Feb 1;458(1):48-56.
[60] Mazur A, Maier JA, Rock E, Gueux E, Nowacki W, Rayssiguier Y. Magnesium and the inflammatory response: potential physiopathological implications. Arch Biochem Biophys. 2007 Feb 1;458(1):48-56.
[61] Mazur A, Maier JA, Rock E, Gueux E, Nowacki W, Rayssiguier Y. Magnesium and the inflammatory response: potential physiopathological implications. Arch Biochem Biophys. 2007 Feb 1;458(1):48-56.
[62] Mazur A, Maier JA, Rock E, Gueux E, Nowacki W, Rayssiguier Y. Magnesium and the inflammatory response: potential physiopathological implications. Arch Biochem Biophys. 2007 Feb 1;458(1):48-56.
[63] Gommers LMM, Goenderop JGJ, Bindels RJM, de Baaij JHF. Hypomagnesemia in type 2 diabetes: a vicious circle? Diabetes. 2016 Jan;65:3-13.
[64] Gropper SS, Smith JL. Advanced nutrition and human metabolism. 6th ed. Belmont (CA): Wadsworth, Cengage Learning; 2013. p. 527-530.
[65] Anderson RA. Chromium, glucose intolerance and diabetes. J Am Coll Nutr. 1998;17(6): 548-555.
[66] Anderson RA. Chromium, glucose intolerance and diabetes. J Am Coll Nutr. 1998;17(6): 548-555.
[67] Anderson RA. Chromium, glucose intolerance and diabetes. J Am Coll Nutr. 1998;17(6): 548-555.
[68] Galland L. Magnesium, stress and neuropsychiatric disorders. Magnes Trace Elem. 1991-1992;10(2-4):287-301.
[69] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[70] Abumaria N, Yin B, Zhang L, Li X-Y, Chen T, Descalzi G, et al. Effects of elevation of brain magnesium on fear conditioning, fear extinction, and synaptic plasticity in the infralimbic prefrontal cortex and lateral amygdala. J Neurosci. 2011 Oct;31(42):14871-14881.
[71] Smith MA. Hippocampal vulnerability to stress and aging: possible role of neurotrophic factors. Behav Brain Res. 1996;78(1):25-36.
[72] Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
[73] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[74] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[75] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[76] Vink R. Magnesium and neurology: new applications for an old friend. Metagenics Congress. June 2016.
[77] Papadopopol V, Nechifor M. Magnesium in neuroses and neuroticism. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:269-281.
[78] Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
[79] Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
[80] Eby GA, Eby KL. Magnesium for treatment-resistant depression: A review and hypothesis. Medical Hypotheses. 2009;74:649-660.
[81] Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
[82] Papadopopol V, Nechifor M. Magnesium in neuroses and neuroticism. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:269-281.
[83] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015:1197-1223.
[84] Manosso LM, Moretti M, Ribeiro CM, Goncalves FM, Leal RB, Rodrigues ALS. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
[85] Manosso LM, Moretti M, Ribeiro CM, Goncalves FM, Leal RB, Rodrigues ALS. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
[86] Manosso LM, Moretti M, Ribeiro CM, Goncalves FM, Leal RB, Rodrigues ALS. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
[87] Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
[88] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1197-1223.
[89] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1202-1213.
[90] Gower-Winter SD, Levenson CW. Zinc in the central nervous system: From molecules to behavior. BioFactors. 2012;38(3):186-193.
[91] Siwek M, Sowa-Kucma M, Styczen K, Szewczyk B, Reczynski W, Misktak, P, et al. Decreased serum zinc concentration during depressive episode in patients with bipolar disorder. J Affect Dis. 2016 Jan;190:272-277.
[92] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1079.
[93] Gropper SS, Smith JL, Groff JL. Advanced nutrition and human metabolism. Belmont (CA): Thomson Wadsworth; 2005. p. 316-321.
[94] Gropper SS, Smith JL, Groff JL. Advanced nutrition and human metabolism. Belmont (CA): Thomson Wadsworth; 2005. p. 316-321.
[95] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1079.
[96] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1079.
[97] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4thed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1079.
[98] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St. Louis (MO): Mosby Elsevier; 2008:306-337.
[99] Vitamin B6 (Pyridoxine; Pyridoxine 5’-phosphate). Altern Med Rev. 2001;6(1):87-92.
[100] Dahle LO, Berg G, Hammar M, Hurtig M, Larsson L. The effect of oral magnesium substitution on pregnancy-induced leg cramps. Am J Obstet Gynecol. 1995;173(1):175-180.
[101] Dahle LO, Berg G, Hammar M, Hurtig M, Larsson L. The effect of oral magnesium substitution on pregnancy-induced leg cramps. Am J Obstet Gynecol. 1995;173(1):175-180.
[102] Roffe C, Sills S, Crome P, Jones P. Randomised, cross-over, placebo controlled trial of magnesium citrate in the treatment of chronic persistent leg cramps. Med Sci Monit. 2002;8(5):CR326-330.
[103] Roffe C, Sills S, Crome P, Jones P. Randomised, cross-over, placebo controlled trial of magnesium citrate in the treatment of chronic persistent leg cramps. Med Sci Monit. 2002;8(5):CR326-330.
[104] Roffe C, Sills S, Crome P, Jones P. Randomised, cross-over, placebo controlled trial of magnesium citrate in the treatment of chronic persistent leg cramps. Med Sci Monit. 2002;8(5):CR326-330.
[105] Kedia S. Complementary and integrative approaches for pediatric headache. Semin Pediatr Neurol. 2016;23:44-52.
[106] Tepper, D. Headache toolbox: Magnesium. Cleveland (OH): American Headache Society; 2013 [cited 2018 Mar 20]. Available from: https://americanheadachesociety.org/wp-content/uploads/2016/06/Magnesium.pdf.
[107] Sun-Edelstein C, Mauskop A. Role of magnesium in the pathogenesis and treatment of migraine. Expert Rev. Neurother. 2009;9(3):369-379.
[108] Alghadeer S. The efficacy of different oral magnesium supplements for migraine prevention: a literature review. Indonesian J Pharm. 2016;27(3):174-182.
[109] Facchinetti F, Sances G, Borella P, Genazzani AR, Nappi G. Magnesium prophylaxis of menstrual migraine: effects on intracellular magnesium. Headache. 1991;31(5):298-301.
[110] Peikert A, Wilimzig, Kohne-Volland R. Prophylaxis of migraine with oral magnesium: results from a prospective, multi-center, placebo-controlled and double-blind randomized study. Cephalalgia. 1996;16:257-263.
[111] Koseoglu E, Talashoglu A, Gonul AS, Kula M. The effects of magnesium prophylaxis in migraine without aura. Mag Res. 2008;21(2):101-8.
[112] Veronese N, Watutantrige-Fernando S, Luchini C, Solmi M, Luchini C, Maggi S. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: a systematic review and meta-analysis of double-blind randomized controlled trials. Eur J Clin Nutr. 2016 Dec;70(12):1463.
[113] Dong J-Y, Xun P, He K, Qin L-Q. Magnesium intake and risk of type 2 diabetes: meta-analysis of prospective cohort studies. Diabetes Care. 2011 Sep;34(9):2116-2122.
[114] Kurstjens S, de Baaij JHF, Bouras H, Bindels RJM, Tack CJJ, Hoenderop JGJ. Determinants of hypomagnesemia in patients with type 2 diabetes mellitus. European Society of Endocrinology. 2017;176(1):11-19.
[115] Dou M, Ma Y, Ma AG, Han L, Song M-M, Wang Y-G, et al. Combined chromium and magnesium decreases insulin resistance more effectively than either alone. Asia Pac J Clin Nutr. 2016;25(4):747-753.
[116] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[117] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[118] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[119] Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
[120] Cernak I, Savid V, Kotur J, Prokic V, Kuljic B, Grbovic D, et al. Alterations in magnesium and oxidative status during chronic emotional stress. Magnes Res. 2000 Mar;13(1):29-36.
[121] Hagmeyer S, Haderspeck JC, Grabrucker AM. Behavioral impairments in animal models for zinc deficiency. Front Behav Neurosci. 2015 Jan;8:443.
[122] Manosso LM, Moretti M, Ribeiro CM, Goncalves FM, Leal RB, Rodrigues ALS. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
[123] Cope EC, Levenson CW. Role of zinc in the development and treatment of mood disorders. Curr Opin Clin Nutr Metab Care. 2010 Nov;13(6):685-689.
[124] Cope EC, Levenson CW. Role of zinc in the development and treatment of mood disorders. Curr Opin Clin Nutr Metab Care. 2010 Nov;13(6):685-689.
[125] Pathak P, Kapil U. Role of trace elements zinc, copper and magnesium during pregnancy and its outcome. Indian J Pediatr. 2004 Nov;71(11):1003-1005.
[126] Long S, Romani AMP. Role of cellular magnesium in human disease. Austin J Nutr Food Sci. 2015 Mar;2(10).
[127] Schulpis KH, Karakonstantakis T, Vlachos GD, Mentis A-FA, Karikas GA, Afordakou D, et al. Maternal-neonatal magnesium and zinc serum concentrations after vaginal delivery. Scand J Clin Lab Invest. 2010 Nov;70(7):465-469.
[128] Long S, Romani AMP. Role of cellular magnesium in human disease. Austin J Nutr Food Sci. 2015 Mar;2(10).
[129] Doll H, Brown S, Thurston A, Vessey M. Pyridoxine (vitamin B6) and the premenstrual syndrome: a randomized crossover trial. J R Coll Gen Pract. 1989;39(326):364-368.
[130] Facchinetti F, Borella P, Sances G, Fioroni L, Nappi RE, Genazzani AR. Oral magnesium successfully relieves premenstrual mood changes. Obstet Gynecol. 1991 Aug;78(2):177-181.
[131] De Souza MC, Walker AF, Robinson PA Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000 Mar;9(2):131-139.
[132] De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000 Mar;9(2):131-139.
[133] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[134] Siebrecht S. Magnesium bisglycinate is a safe form of mineral supplementation in human nutrition. International Journal of Orthomolecular and Related Medicine. 2013:144.
[135] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 24]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[136] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[137] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[138] National Kidney Foundation [Internet]. New York: National Kidney Foundation; Are Magnesium supplements harmful to the kidneys? 2013 Oct 8. [cited 2018 Feb 1]. Available from: https://www.kidney.org/blog/ask-doctor/are-magnesium-supplements-harmful-kidneys.
[139] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 3]. Available from: http://www.naturaldatabase.com. subscription required to view.
[140] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[141] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Oct 18th]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[142] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 556.
[143] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p. 232.
[144] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[145] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 3]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[146] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[147] Medline Plus U.S. National Library of Medicine. Dasatinib [Internet]. Bethesda. 2016 Aug 8 [cited 2017 Nov 3]. Available from: https://medlineplus.gov/druginfo/meds/a607063.html
[148] Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 84-85.
[149] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 556.
[150] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 3]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[151] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p. 137-8.
[152] Michigan Medicine University of Michigan. Hydroxychloroquine [Internet]. Michigan. 2015 Mar 3 [cited 2017 Nov 6]. Available from: http://www.uofmhealth.org/health-library/hn-1141007.
[153] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[154] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 24]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[155] Vitamin B6. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Dec 19]. Available from: http://www.naturaldatabase.com. subscription required to view.
[156] Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 270-1.
[157] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2008 [cited 2021 Feb 22]. Available from: http://www.naturaldatabase.com. subscription required to view.
[158] Kashihara Y, Terao Y, Yoda K, Hirota T, Kubota T, Kimura M, Matsuki S, Hirakawa M, Irie S, Ieiri I. Effects of magnesium oxide on pharmacokinetics of L-dopa/carbidopa and assessment of pharmacodynamic changes by a model-based simulation. Eur J Clin Pharmacol. 2019 Mar;75(3):351-361. doi: 10.1007/s00228-018-2568-4. Epub 2018 Oct 31. PMID: 30382297.
[159] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 557.
[160] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[161] Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 180.
[162] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p.190.
[163] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p.190.
[164] Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 201.
[165] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p. 11.
[166] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 574.
[167] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 574.
[168] Zinc. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [updated 2017 Dec 21; cited 2018 Feb 20]. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx?productid=982. Subscription required to view.
[169] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 640-641.
[170] Vitamin B6. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2018 Jan 8]. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx?productid=934. Subscription required to view.
[171] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney AU): Elsevier/Churchill Livingstone; 2015. p. 1078-1091.
[172] Vitamin B6. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2018 Jan 8]. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx?productid=934. Subscription required to view.
[173] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1078-1091.
[174] Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 169.
[175] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p. 8.
[176] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 3]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[177] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[178] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 557.
[179] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[180] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 3]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[181] Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 241-242.
[182] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p.179.
[183] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[184] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 3]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[185] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1218.
[186] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p. 179.
[187] Oregon State University - Linus Pauling Institute [Internet]. Corvallis (OR): Linus Puling Institute; c2002-2018. Micronutrient information centre - zinc; 2001 [2013 Jun; cited 2018 Jan 9]. Available from: http://lpi.oregonstate.edu/mic/minerals/zinc.
[188] Zinc. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [updated 2017 Dec 12; cited 2018 Jan 9]. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx?productid=982. Subscription required to view.
[189] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[190] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [2017 Oct 30]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[191] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 557.
[192] Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 241-242.
[193] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p.179.
[194] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 688-9.
[195] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Nov 3]. Available from: http://www.naturaldatabase.com. Subscription required to view.
[196] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1218.
[197] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p. 179.
[198] Oregon State University - Linus Pauling Institute [Internet]. Corvallis (OR): Linus Puling Institute; c2002-2018. Micronutrient information centre - zinc; 2001 [2013 Jun; cited 2018 Jan 9]. Available from: http://lpi.oregonstate.edu/mic/minerals/zinc.
[199] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 618-652.
[200] Zinc. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [updated 2017 Dec 12; cited 2018 Jan 9]. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx?productid=982. Subscription required to view.
[201] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p.281.
[202] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 557.
[203] Zinc. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [updated 2017 Dec 12; cited 2018 Jan 9]. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx?productid=982. Subscription required to view.
[204] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1197-1223.
[205] Vitamin B6. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2018 Jan 8]. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx?productid=934. Subscription required to view.
[206] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 312-313.
[207] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1078-1091.
[208] Magnesium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Oct 18th]. Available from: http://www.naturaldatabase.com. subscription required to view.
[209] Ravn HB, Vissinger H, Kristensen SD, Wennmalm A, Thygesen K, Husted SE. Magnesium inhibits platelet activity--an infusion study in healthy volunteers. Thromb Haemost. 1996 Jun;75(6):939-44.
[210] Chromium. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 March 9]. Available from: http://www.naturaldatabase.com. subscription required to view.
[211]Braun L, Cohen L. Chromium In: Herbs & natural supplements: an evidence-based guide. 4th Edition. Sydney: Elsevier/Churchill Livingstone. 2015. p.180-90.
Vitamin B6. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2018 [cited 2017 Dec 19]. Available from: http://www.naturaldatabase.com. subscription required to view.
Harkness R, Bratman S. Mosby’s handbook of drug-herb and drug-supplement interactions. St Louis (MO): Mosby Inc.; 2003. p. 270-1.
[212] Gaby AR, Batz F, Chester R, Constantine G. A-Z guide to drug-herb-vitamin interactions. 2nd ed. New York (NY): Three Rivers Press; 2006. p. 180-1.
[213] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 556.
[214] Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney (AU): Elsevier/Churchill Livingstone; 2015. p. 1218.
[215] Stargrove MB, Treasure J, McKee DL. Herb, nutrient, and drug interactions. St Louis (MO): Mosby Elsevier; 2010. p. 618-652.
[216] National Health and Medical Research Council. Nutrient Reference Values for Australia and New Zealand. Chromium [Internet]. Canberra (ACT): Australian Government. 2014 Mar 9. [2021 Apr 30]. Available from: https://www.nrv.gov.au/nutrients/chromium.
WARNINGS
Cautions and Contraindications
Contraindications
Heart block: For patients with heart block, which involves the heart beating too slowly, one source states that intravenous magnesium is contraindicated.[135] Another source states that magnesium supplements should be avoided also.[136]
Kidney disease, severe: For patients with severe kidney disease, taking magnesium supplements may increase the risk of hypermagnesaemia, therefore avoid in this group.[137],[138]
Moderate Level Cautions
Aminoglycoside antibiotics: Magnesium may form insoluble complexes with some aminoglycoside antibiotics, which could reduce their absorption. Separate doses by at least 2 hours.[139],[140]
Bisphosphonates: Magnesium may form insoluble complexes with this medication, reducing absorption. The bisphosphonates include alendronate (Fosamax), etidronate (Didronel), ibandronate (Boniva), risedronate (Actonel), and tiludronate (Skelid), and others.[141],[142],[143] Separate doses by at least 2 hours.
Calcium-channel blockers: Magnesium inhibits calcium entry into smooth muscle cells and may therefore theoretically have additive effects with calcium channel blockers, potentially resulting in hypotension and neuromuscular weakness. These drugs include nifedipine (Adalat, Procardia), nicardipine (Cardene), isradipine (DynaCirc), amlodipine (Norvasc), and others.[144],[145] Monitor this combination closely and adjust medication doses as required.
Dasatinib: Dasatinib is a medication used primarily to treat different types of leukemia. There is mixed information about the use of this drug with magnesium. One source states that this drug may increase magnesium blood levels.[146] Other sources state that magnesium hydroxide products reduce Dasatinib’s absorption and therefore should not be taken with Dasatinib.[147] If a patient is taking Dasatinib and any form of magnesium, it is best to separate doses by at least 2 hours, and monitor closely.
Digoxin: There is evidence that magnesium and digoxin may chelate, reducing absorption and bioavailability of both. Therefore, digoxin and magnesium supplements should be administered at least 2 hours apart.[148],[149],[150]
Hydroxychloroquine: Hydroxychloroquine is an antimalarial drug, used to prevent and treat acute attacks of malaria, as well as to treat both acute and chronic rheumatoid arthritis and lupus. Magnesium supplementation may reduce blood levels of chloroquine, a compound similar to hydroxychloroquine, and decrease its effectiveness. Until more is known, it is suggested that those people taking hydroxychloroquine for arthritis, who are also using magnesium supplements and are not experiencing relief, might take them at separate times.[151],[152]
Kidney disease, compromised, not severe: For patients with compromised kidney function, taking magnesium supplements may increase the risk of hypermagnesaemia. Use cautiously and monitor closely in this group of patients.[153],[154]
Levodopa: Vitamin B6 at doses of 5 to 25 mg and above may enhance the metabolism of levodopa, reducing its anti-parkinsonism effects. Monitor patients when combining.[155],[156] Further, magnesium may reduce the bioavailability of levodopa.[157] A pharmacokinetic interaction study of magnesium and levodopa found that 1g of magnesium oxide was shown to significantly reduce the bioavailability of levodopa by 80.9% in healthy volunteers.[158] Closely monitor those who are taking supplemental magnesium alongside levodopa and separate dosing by at least two hours.
Neuromuscular blocking agents: Magnesium can increase and prolong agent effects. This has been seen in patients receiving magnesium intravenously. Unintentional additive effects may be detrimental, however, intentional co-administration may result in a reduced requirement for the neuromuscular blocking agent. Therefore monitor this combination closely.[159],[160]
Nitrofurantoin: Nitrofurantoin is an antibiotic used to treat bladder infections. Magnesium supplements may interfere with the absorption of nitrofurantoin.[161],[162] The mechanism for this is unclear. In one study, nitrofurantoin absorption was reduced by also taking magnesium tisilicate, an antacid. In another, magnesium was shown to bind with nitrofurantoin in a test tube.[163]
Penicillamine:Magnesium may reduce the absorption of penicillamine, causing it to be less effective.[164],[165],[166] Penicillamine is thought to form complexes with magnesium, reducing magnesium absorption and also reducing its own availability.[167] Therefore separate doses by at least two hours.
Zinc forms an insoluble complex with penicillamine, which interferes with absorption and activity, and reduces the bioavailability of both substances.[168],[169] Therefore, it is recommended to separate doses by 2 hours.
Phenobarbitone (phenobarbital): At doses above 200 mg daily, vitamin B6 can reduce plasma levels of this anticonvulsant. High doses of vitamin B6 should therefore be avoided in people on this medication.[170],[171] Consider the patient’s total daily intake.
Phenytoin: At doses above 200 mg daily, Vitamin B6 can reduce plasma levels of this anticonvulsant. High doses of vitamin B6 should be avoided in people on this medication.[172],[173] Consider the patient’s total daily intake.
Potassium-sparing diuretics: Animal studies show that potassium-sparing diuretics could reduce urinary excretion of magnesium. This could create a risk of hypermagnesemia.[174],[175],[176],[177] The potassium-sparing diuretics include amiloride (Midamor), triamterene (Dyrenium), spironolactone (Aldactone) and others. Use caution with this combination.
Quinolone antibiotics:When magnesium is taken with quinolone antibiotics, it may reduce their absorption.[178],[179],[180], [181],[182] To avoid this interaction, it is advised to separate doses by at least two hours before, or four hours after oral magnesium.[183],[184] Some quinolone antibiotics include ciprofloxacin (Cipro), levofloxacin (Levaquin), ofloxacin (Floxin), moxifloxacin (Avelox), gatifloxacin (Tequin), and others.
These antibiotics may form complexes when taken with zinc, reducing the efficacy of both the antibiotic and zinc supplement. Therefore, it is recommended to separate doses by taking the medication 2 hours before, [185],[186],[187] or four to six hours after zinc.[188]
Tetracycline antibiotics:When magnesium is taken with tetracycline classes of antibiotics, it may reduce their absorption.[189],[190],[191], [192],[193] To avoid this interaction, it is advised to separate doses by at least two hours before, or four hours after oral magnesium.[194],[195]
These antibiotics may form complexes when taken with zinc, reducing the efficacy of both the antibiotic and zinc supplement. Therefore, it is recommended to separate doses by taking the medication two hours before,[196],[197],[198] or four to six hours after zinc.[199],[200]
Warfarin: Warfarin may bind with magnesium when taken at the same time, decreasing both warfarin and magnesium’s absorption and activity. People on warfarin therapy should take warfarin and magnesium supplements at least 2 hours apart.[201],[202]
Low Level Cautions
Amiloride: This thiazide and potassium-sparing diuretic has conflicting information regarding a potential interaction with zinc. Amiloride has been reported to lead to zinc deficiency, and also to reduce zinc excretion, leading to zinc accumulation. Monitor zinc status.[203],[204]
Amiodarone: Conflicting information exists regarding potential interactions between amiodarone and vitamin B6. Preliminary research suggests that vitamin B6 can exacerbate amiodarone-induced photosensitivity. Other research suggests a protective effect.[205],[206] Monitor patients for signs of photosensitivity.[207]
Anticoagulants/antiplatelets: Magnesium may affect blood coagulation, and when taken with anticoagulant medications, may increase the risk of bleeding. The evidence for this so far has only been seen in vitro and with infusions.[208],[209] Monitor if patients are taking this combination.
Insulin and other hypoglycaemic medications: Chromium may have insulin sensitising effects and may reduce the requirement for hypoglycaemic medications, consequently increasing the risk of hypoglycaemia as well. Interaction may be beneficial, but individuals should continue to monitor their blood glucose.[210],[211]
Misoprostol: Misoprostol is a prostaglandin E1 analog that protects the mucosal lining of the stomach and intestines. A common side effect of the drug is diarrhoea, which is aggravated by taking magnesium.[212],[213] Consequently, individuals who experience diarrhoea while taking misoprostol should be cautious and monitor dosing of magnesium.
Nonsteroidal anti-inflammatory drugs (NSAIDs): Zinc may form insoluble complexes with certain NSAIDs. Separate doses by at least 2 hours.[214],[215]
Pregnancy and Breastfeeding
Pregnancy: Caution.Safety has not been conclusively established during pregnancy. Practitioner discretion is advised when prescribing for use in pregnancy due to the following cautions:
The upper tolerable limit of chromium a day has not been established due to insufficient data. Consider total chromium intake from diet and supplements compared to the RDI.[216]
Breastfeeding: Appropriate for use.
MGXCALXTS